Exocrine pancreatic insufficiency (EPI)
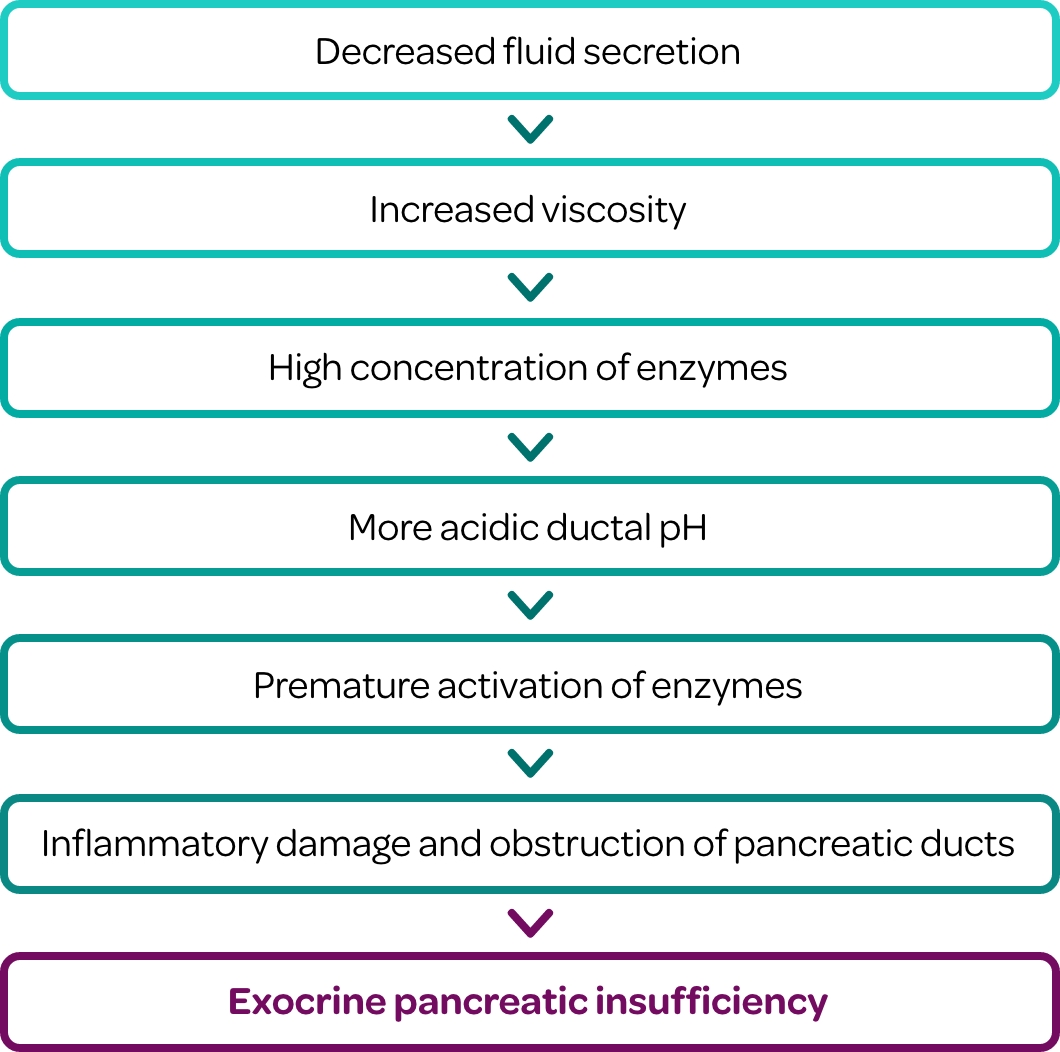
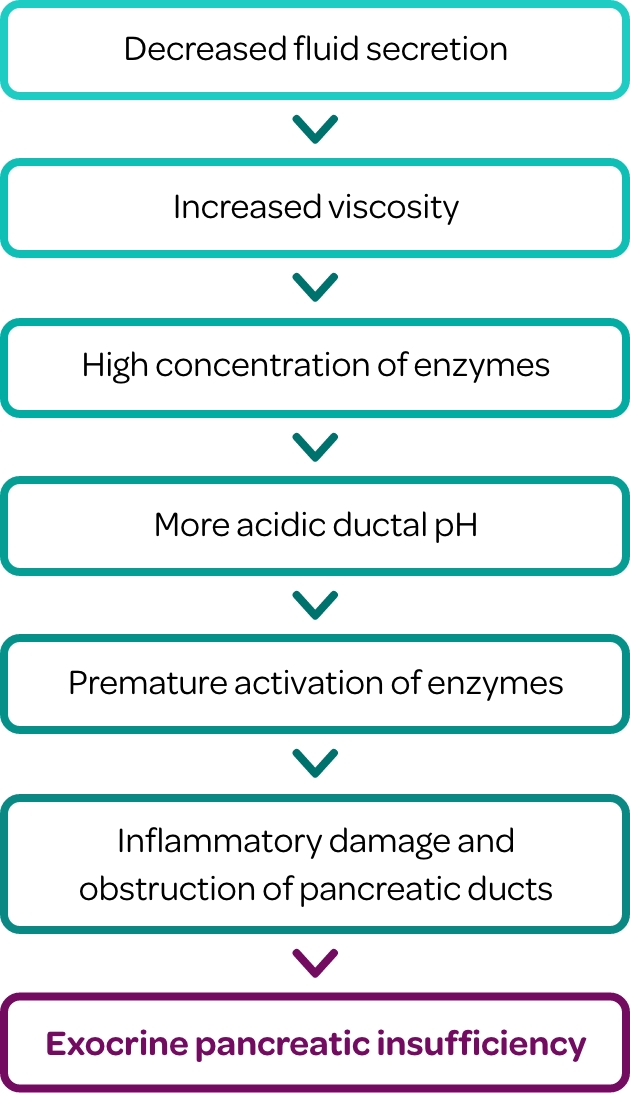
EPI is a condition that is caused by reduced production, delivery, or activity of pancreatic enzymes, leading to impaired digestion, inadequate nutrient absorption, and diminished quality of life.1-3 Essentials of EPI is a curated library of:
Educational Materials
Clinical Tools
Medical Insights
Peer Stories
Find resources that are most meaningful to you.
Choose your medical specialty:
Are you most interested in information and resources related to:
Are you most interested in information and resources related to:
Are you most interested in information and resources related to:
Are you most interested in information and resources related to:
Are you most interested in information and resources related to:
Are you most interested in information and resources related to:
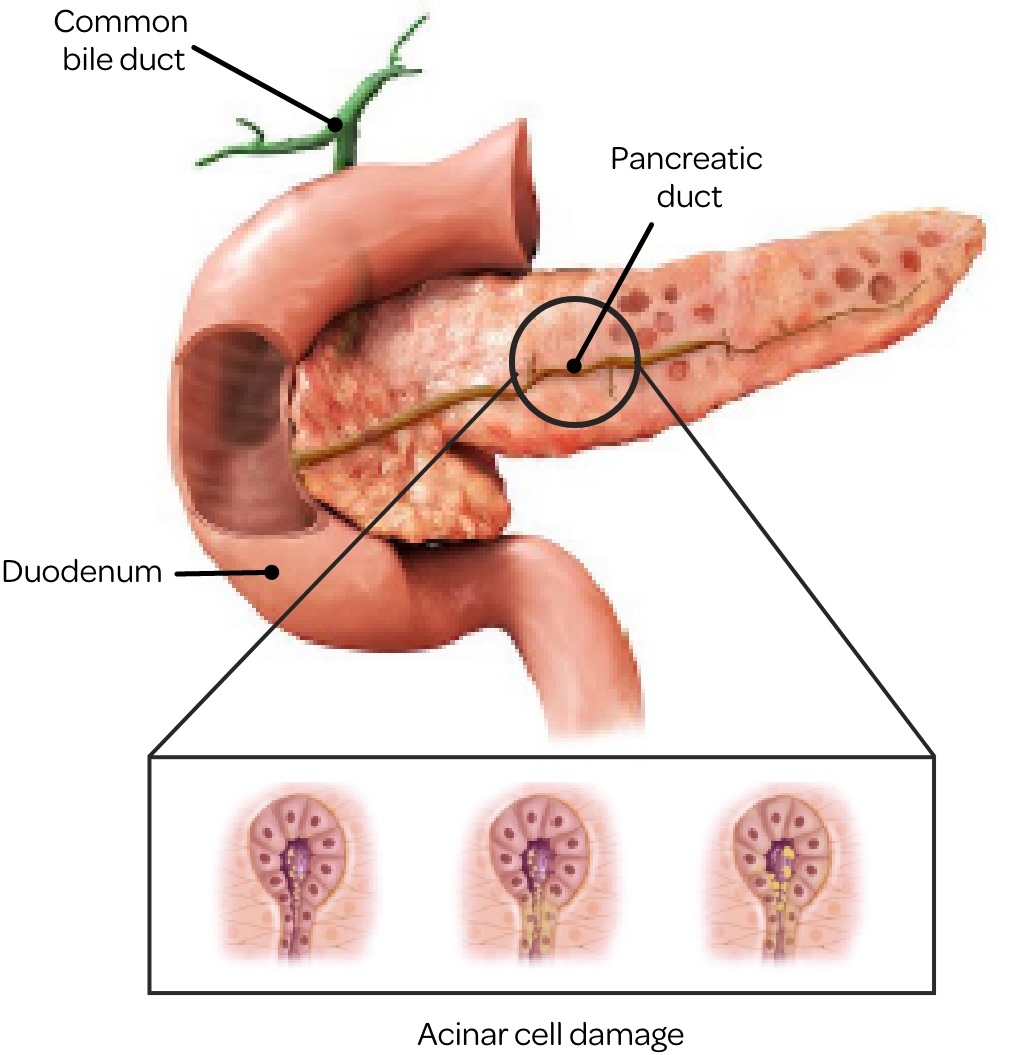
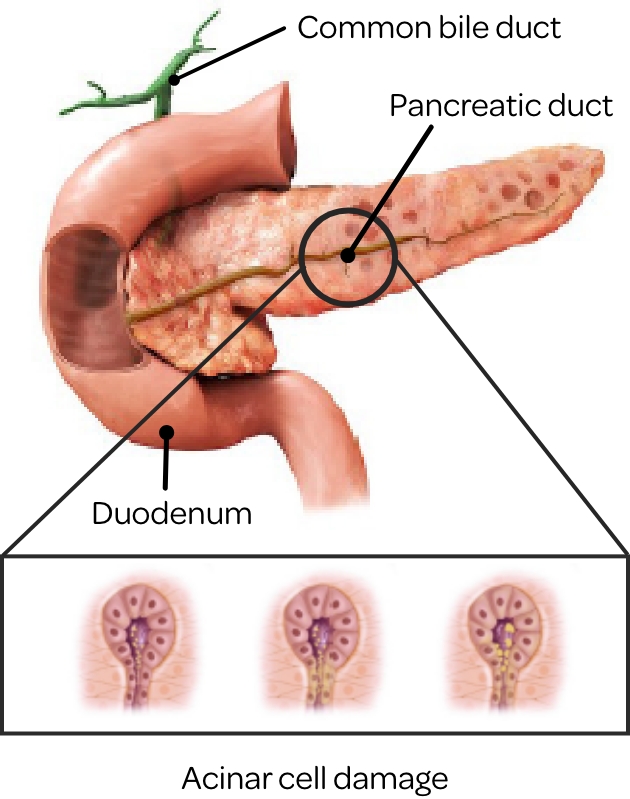
Understanding EPI

 If someone is experiencing ongoing GI issues,
If someone is experiencing ongoing GI issues,
it could be the result of EPI.
EPI limits the pancreas’ ability to break down food,
resulting in uncomfortable symptoms:4
- Frequent gas and/or abdominal bloating
- Unexplained stomach pains
- Frequent diarrhea
- Foul-smelling, greasy stools
EPI is often under recognized due to lack of awareness and is commonly misdiagnosed with
gastrointestinal conditions due to overlapping symptoms.4-9
According to the EPI Uncovered survey:10
66% of patients
have never heard of EPI
78% of patients
are not aware of EPI signs
and symptoms
34% of GI physicians
report EPI is not top of their
differential diagnosis for patients
with complaint of diarrhea
The EPI Uncovered survey was conducted online by Harris Poll on behalf of the American Gastroenterological Association (AGA) and was sponsored by AbbVie. It included 1,001 adults who have experienced at least two GI issues three or more times in the past three months (“patients”) and 500 HCPs, including 250 primary care physicians and 250 gastroenterologists.
Understanding the Patient Experience:
The Diagnostic Journey of Exocrine Pancreatic Insufficiency
What Is the Prevalence of EPI?
EPI is a highly prevalent, chronic digestive disorder that has a significant impact on patients’ lives. The exact prevalence of EPI in the United States is unknown.
Studies show that EPI affects:
Up to 90% of patients
with cystic fibrosis11
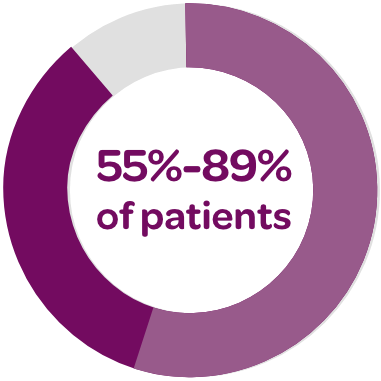
30%-90% of patients
with chronic pancreatitis12*
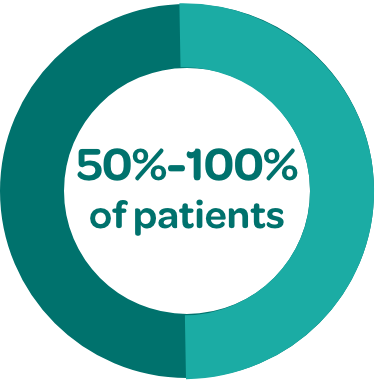
50%-100% of patients
with pancreatic cancer13†
27%-35% of patients with
acute pancreatitis14,15‡
4%-80% of patients with
celiac disease16
39% and 28% of
patients with T1DM§ and
T2DM,∥ respectively17,18
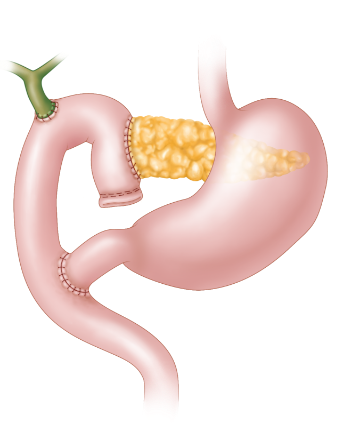
Additional underlying conditions in which EPI has been reported include IBS-D, ulcerative colitis, Crohn’s disease, and gastric surgery.16
Patient Factors That May Delay Diagnosis
EPI Uncovered survey showed that:10

Patients hesitate to
address GI symptoms
Patients wait nearly 4 years to see a doctor about their GI symptoms on average.

Why do they wait?
3 out of 5 patients who found it difficult to discuss symptoms with their HCP said it was due to embarrassment.

What do they do instead?
Patients try to self-manage their GI symptoms by eating healthier (60%) and/or researching symptoms or self‑diagnosing their condition (50%).
Patient-Provider Communication Is Critical
Partnering with patients who are at risk for EPI by encouraging them to communicate transparently about any symptoms they are experiencing can lead to early diagnosis and prompt management.
Questions for Clinical Consideration:
- Have you noticed a change in your bowel habits including greasy stools, frequent loose or watery stools?
- Have you changed your diet in response to GI symptoms?
- Have you experienced unintentional weight loss?
- Do you experience excessive gas or bloating?
- Have you reduced your portion sizes because you are uncomfortable after eating?
Diagnostic Discussions: A Patient’s Perspective

Test your knowledge of EPI
Join us for an interactive, fun, self-paced JEOPARDY!® game to learn more about EPI!
PLAY THE EPI GAME
Want to have an in-person hosted game at your office or
institution?
Contact your MSL and schedule a day to play!