Clinical Overview
What is Exocrine Pancreatic Insufficiency (EPI)?
EPI is a condition characterized by the deficiency of exocrine pancreatic enzymes below the threshold required for normal digestion and is associated with morbidity and reduced quality of life.1,2
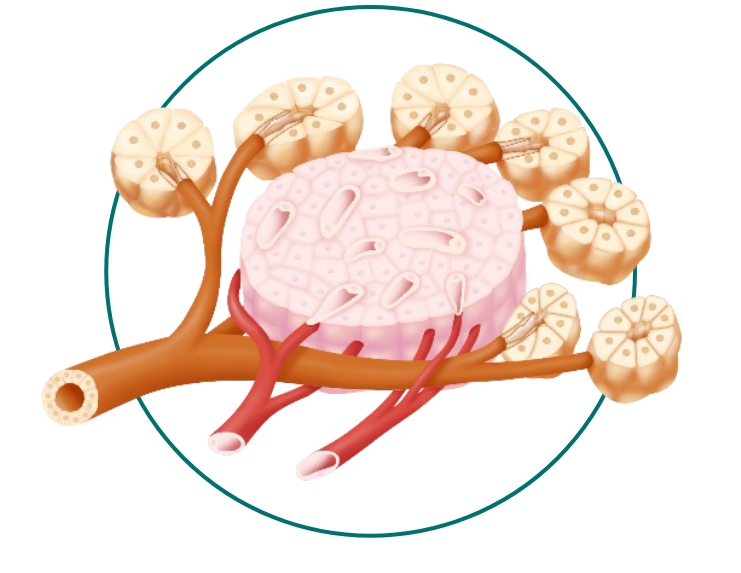
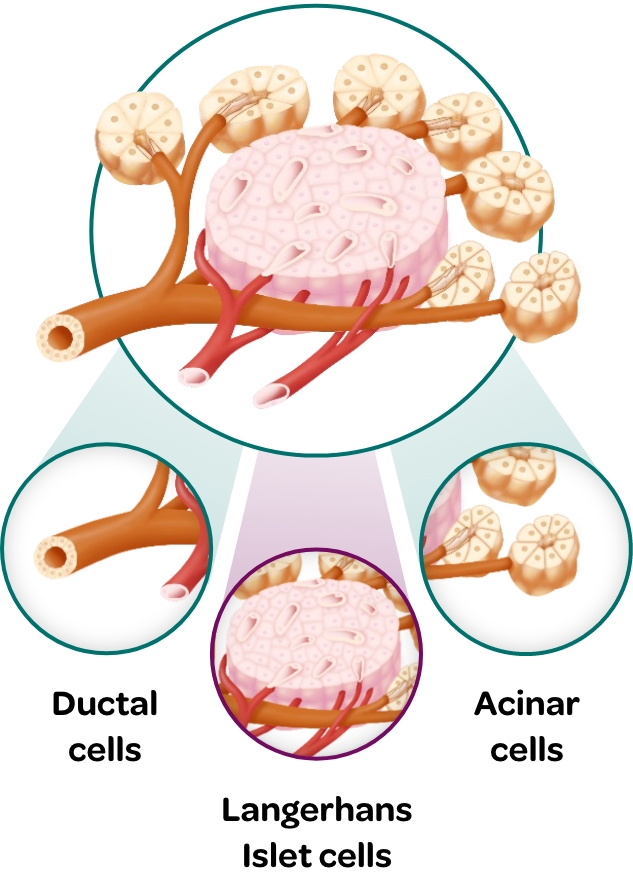
Physiology of the Pancreas
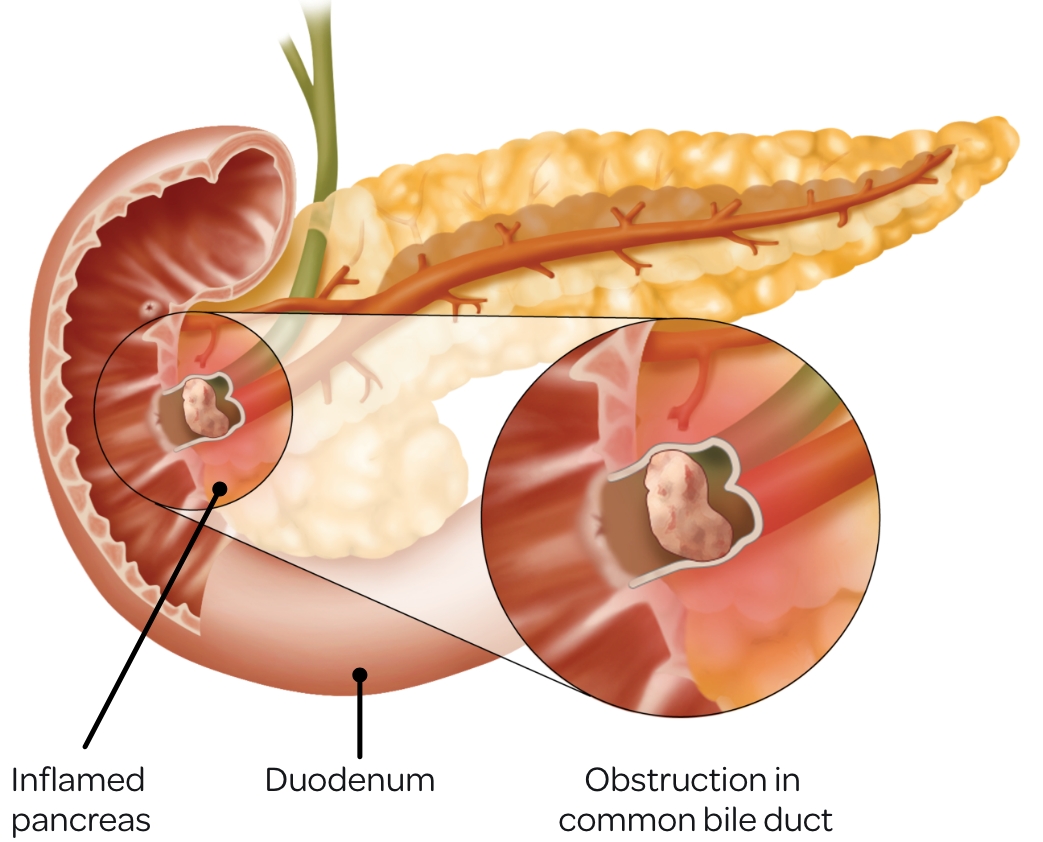
The pancreas is a dual-function gland with:Exocrine Function Plays a pivotal role in digestive physiology by synthesizing and releasing digestive enzymes into the duodenum:
- Contributes significantly to nutrient metabolism and overall nutritional well-being4
Endocrine Function Plays a crucial role in glucose homeostasis3 by producing and releasing hormones into the bloodstream:
Insulin
Glucagon
Somatostatin
Somatostatin
- Inhibits endocrine secretion, particularly insulin and glucagon, thus modulating glucose homeostasis
- Reduces gastrointestinal motility and delays gastric emptying, impacting nutrient absorption
- Modulates the secretion of other hormones like growth hormone and thyroid-stimulating hormone
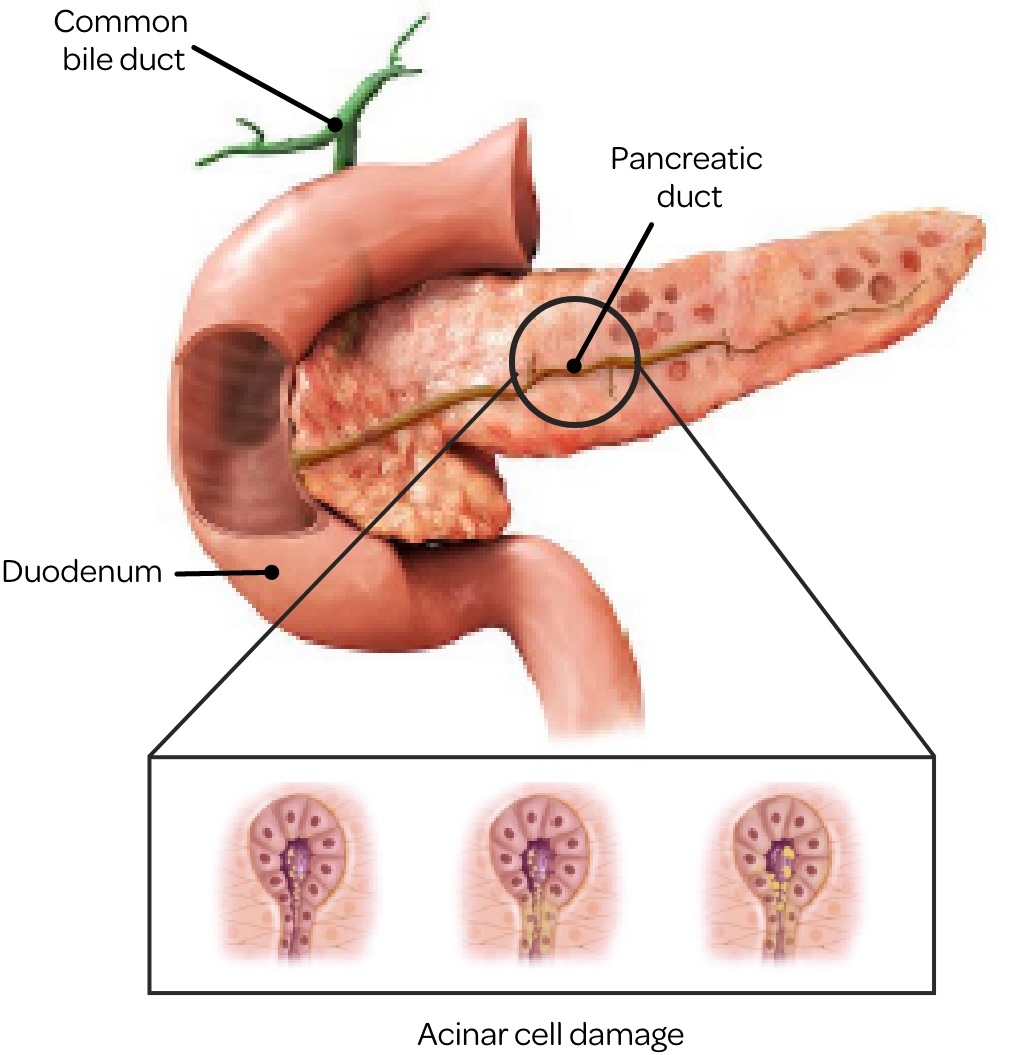
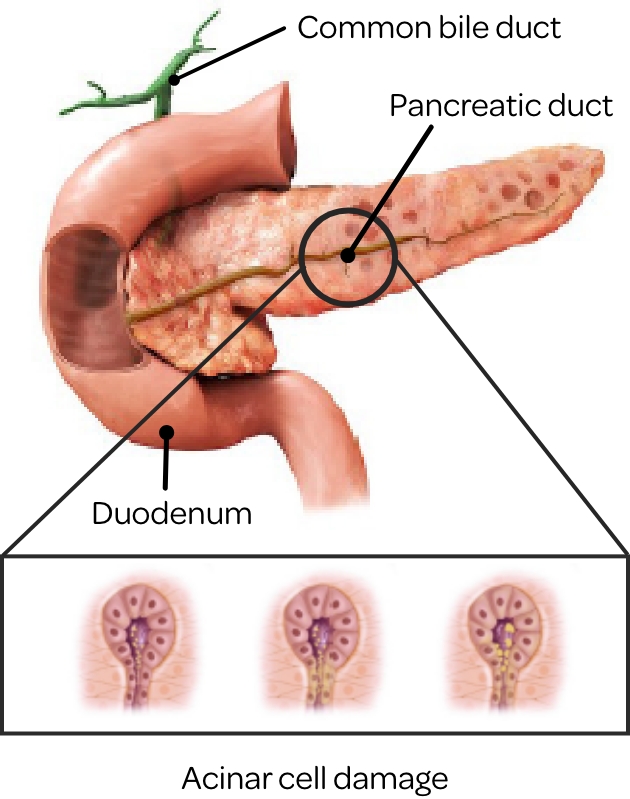
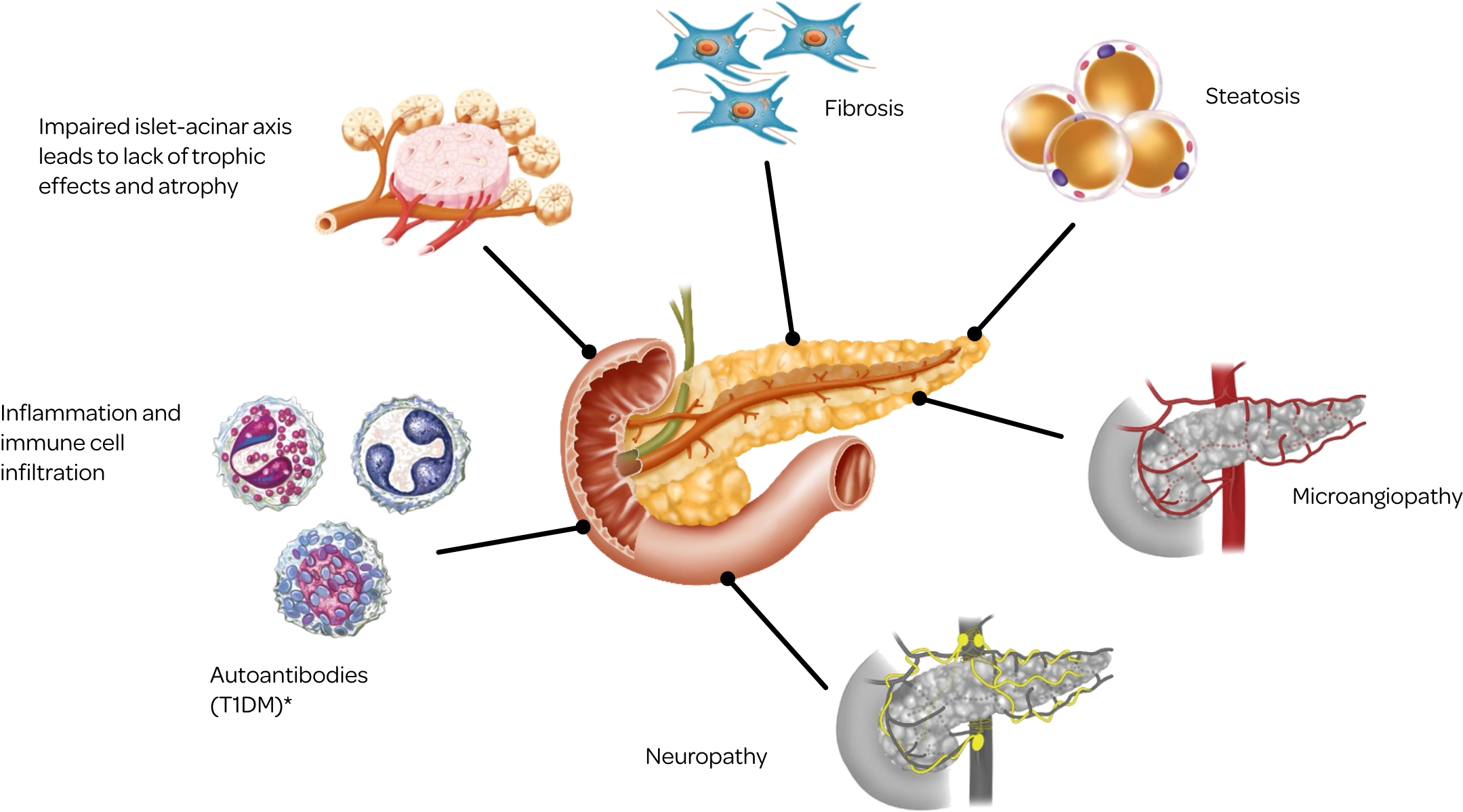
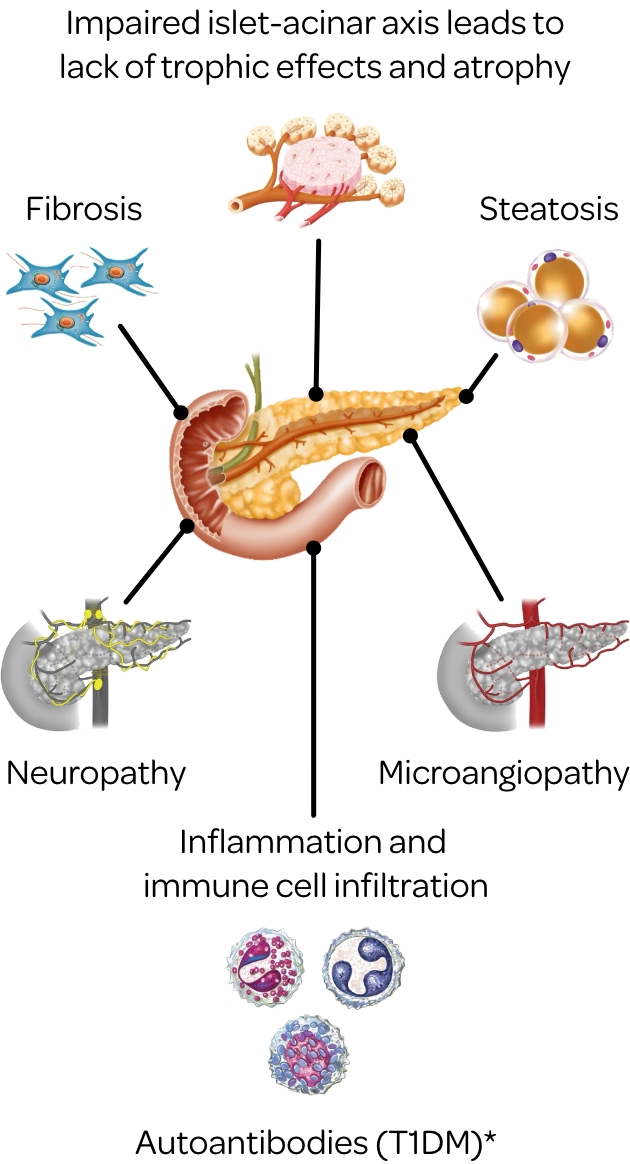
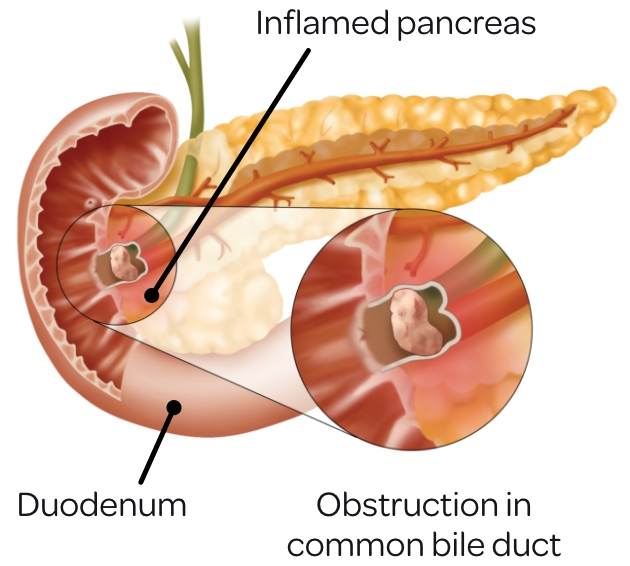
Pathophysiology
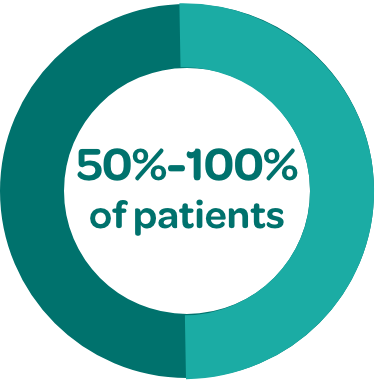
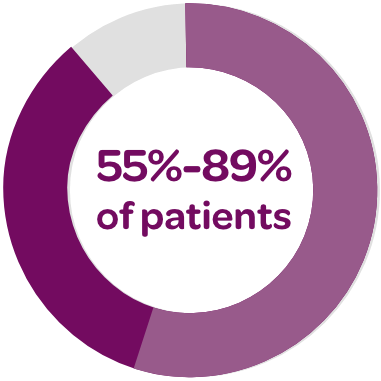
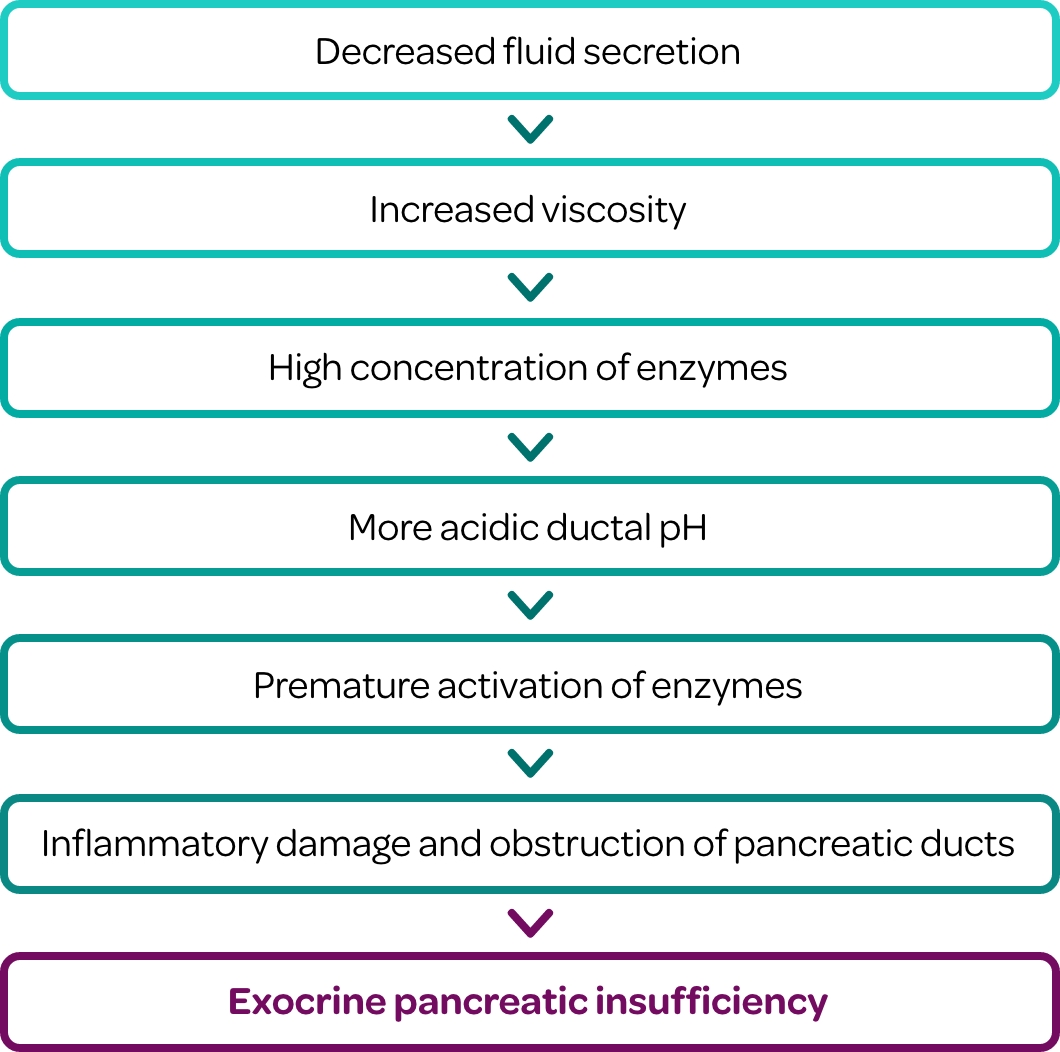
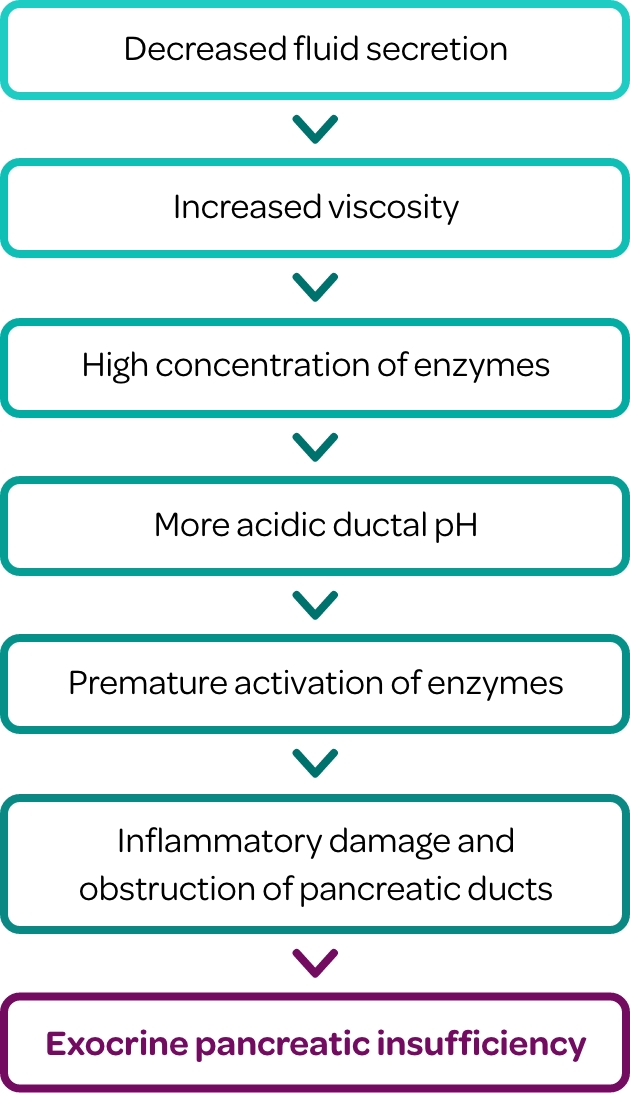
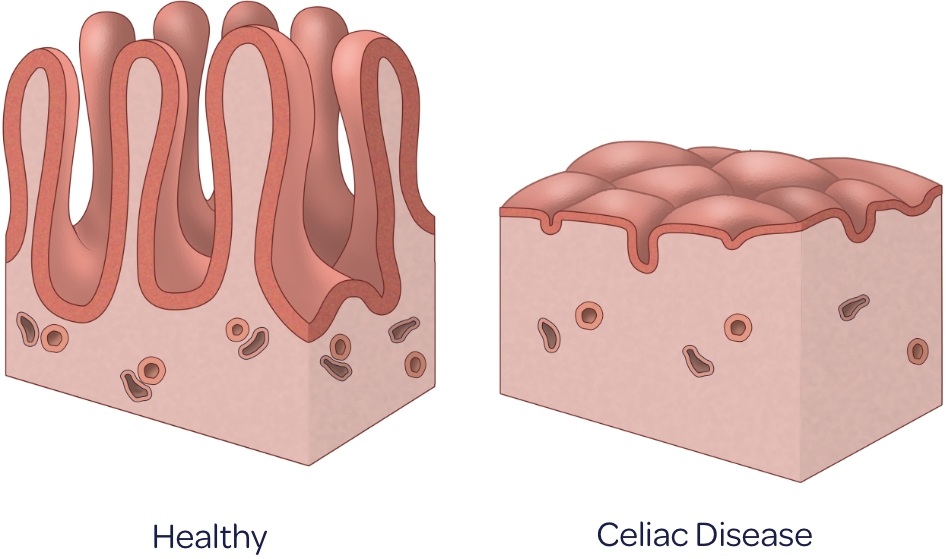
In individuals affected with EPI there is a reduction in pancreatic enzyme production, delivery and/or activity to a level below the threshold required to maintain normal digestion.1
Decreased Production2
Loss of pancreatic parenchyma
Impaired hormonal stimulation
Decreased Activity2*
Poor mixing of pancreatic
enzymes, postprandial
asynchrony, low duodenal pH
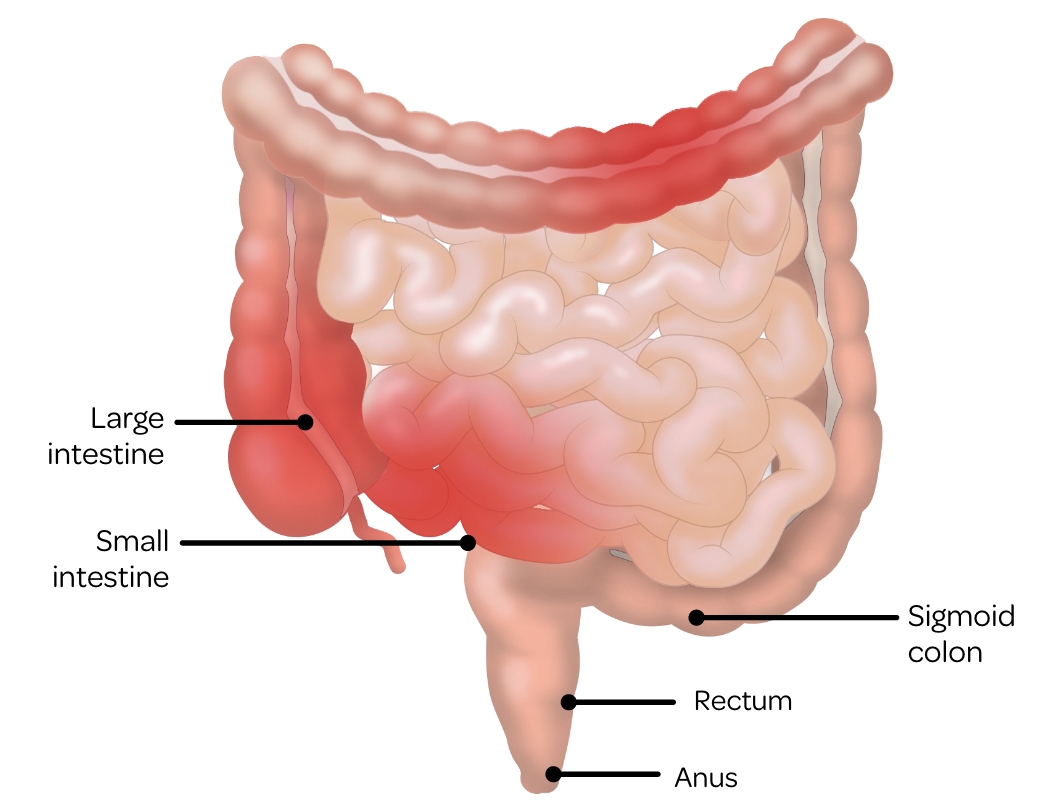
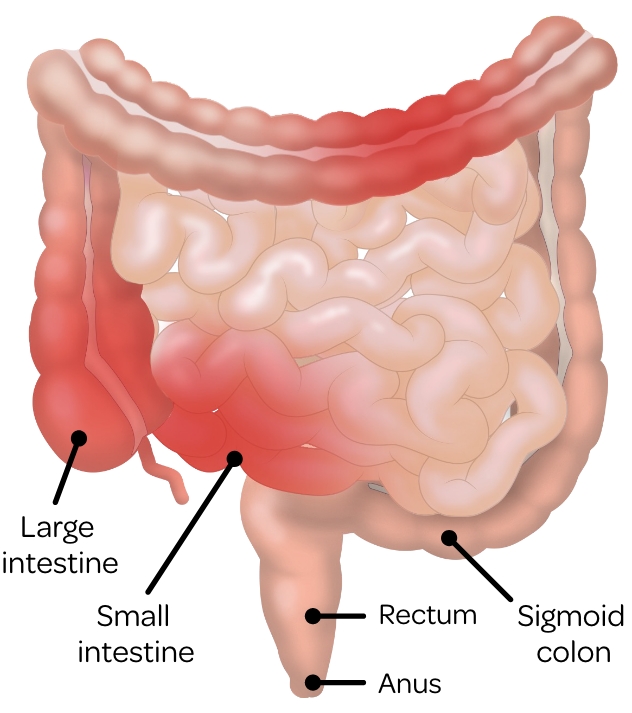
This inadequacy impairs the effective digestion of dietary carbohydrates, fats, and proteins in the small intestine.1 When partially digested food reaches the colon, it may produce symptoms such as osmotic diarrhea and steatorrhea.6
Abdominal pain/discomfort, flatulence, and bloating can also arise partly due to bacterial fermentation, which converts undigested nutrients to short-chain fatty acids for energy.6-8
Take an immersive journey into the physiology of the
exocrine pancreas and the pathophysiology of EPI.
How Does EPI Manifest?
Clinical features of EPI are usually nonspecific and can include:9
What Are the Clinical Manifestations of EPI?
Malabsorption and nutritional deficiencies can reduce quality of life and increase the risk of:1,10-12
Watch this video to see the clinical consequences of EPI
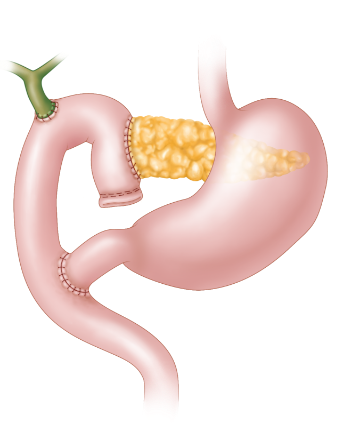
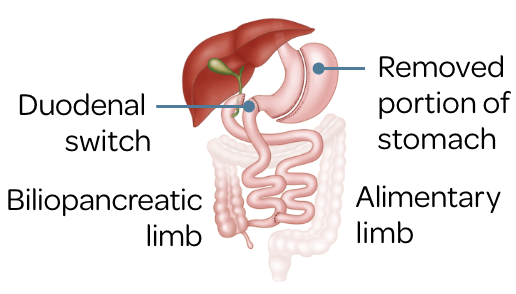
Underlying Conditions and Procedures
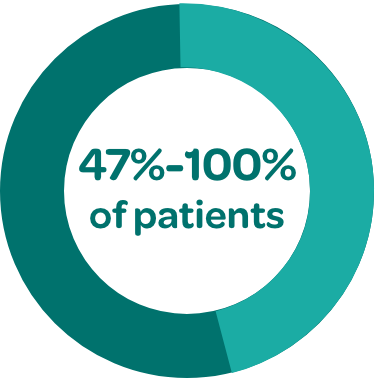
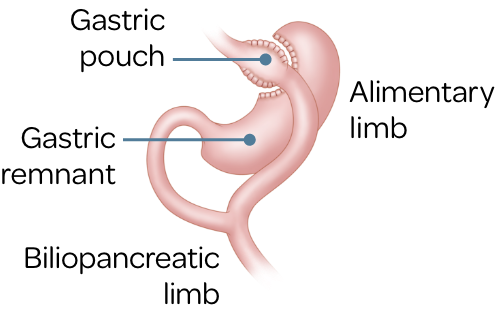
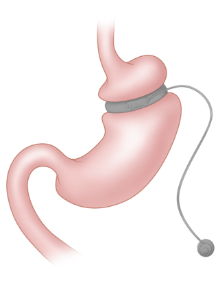
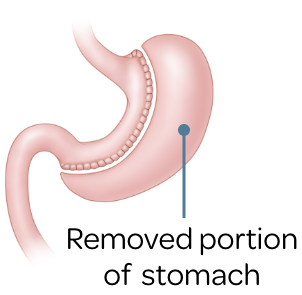
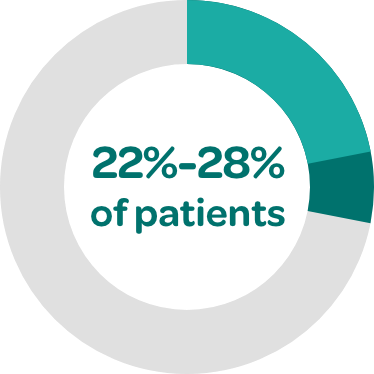
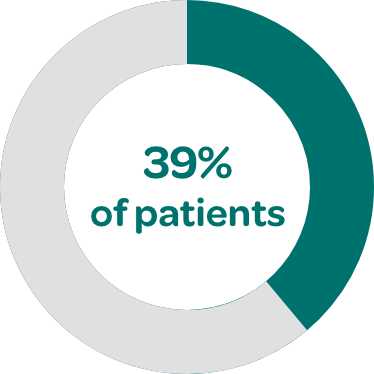
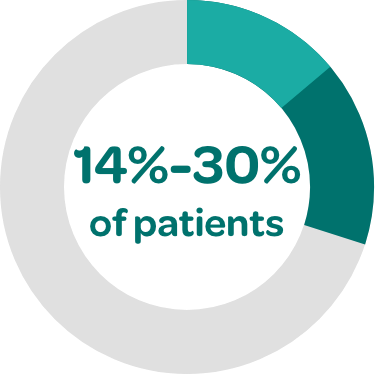
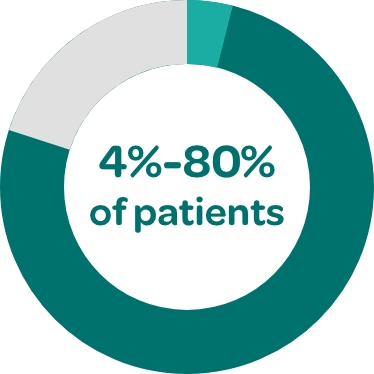
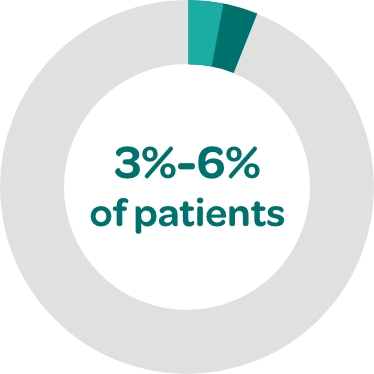
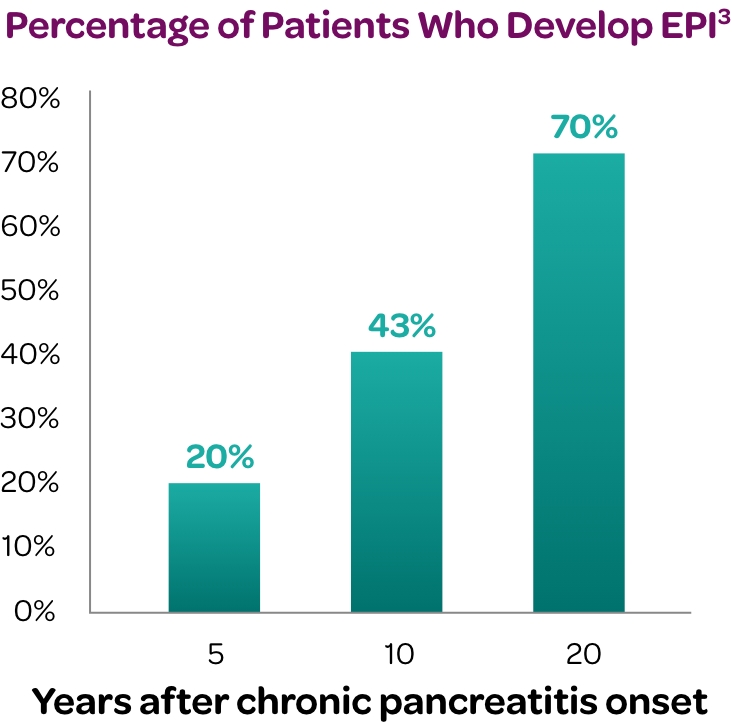
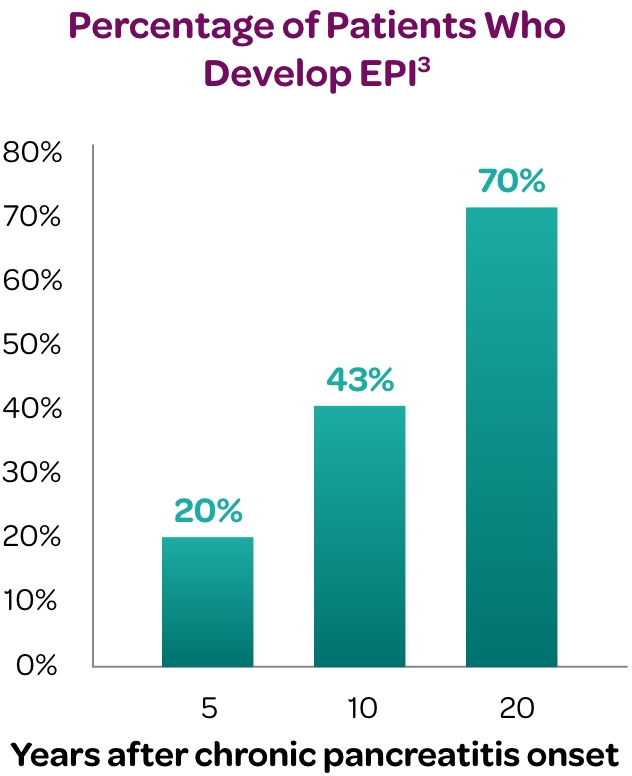
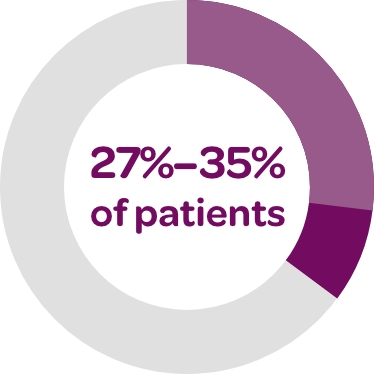
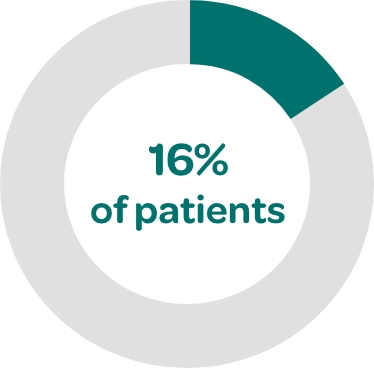
Any disease that significantly damages the pancreatic tissue can cause EPI. In addition, EPI can be a consequence of secondarily impaired exocrine pancreatic function.