Many Faces of EPI: Celiac
Learn about what can cause EPI in patients with celiac disease.
Transcript
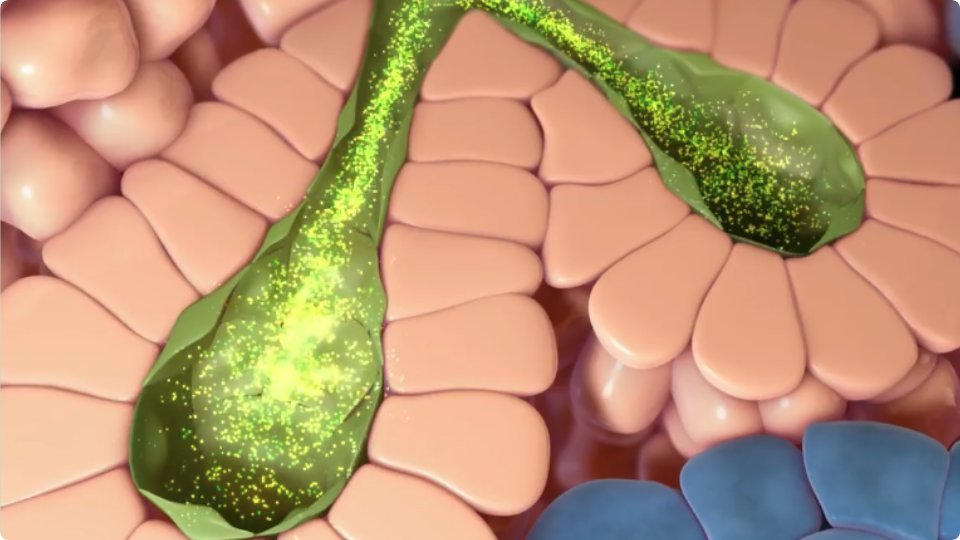
Hello, I’m Dr. Kofi Clarke – I’m a board-certified gastroenterologist specializing in inflammatory bowel diseases and celiac disease. I will be discussing the etiology and pathophysiology of exocrine pancreatic insufficiency in certain patients with celiac disease. Exocrine pancreatic insufficiency (or EPI) may result from many underlying conditions including, but not limited to, chronic or acute pancreatitis, pancreatic surgery, or celiac disease. Causes of persistent gastrointestinal symptoms in patients with celiac disease include suboptimal compliance with a gluten free diet, microscopic colitis, bacterial overgrowth syndrome, IBS, brush border enzyme deficiency, refractory celiac disease and EPI which is often overlooked. Studies utilizing fecal elastase testing show EPI may be a common comorbidity of patients with celiac disease. EPI, is caused by inadequate production, delivery, or activity of pancreatic digestive enzymes leading to insufficient digestion of food, and therefore, malnourishment. During functional digestion, nutrients entering the duodenum trigger the release of hormones such as cholecystokinin, or CCK, which are required for the stimulation of digestive enzymes from the acinar cells in the pancreas. These enzymes are required for the breakdown of food and absorption of nutrients. In celiac disease, endocrine cells in the duodenal mucosa can be damaged by the body’s auto immune response, resulting in decreased levels of CCK. This reduced stimulation of vital digestive enzyme from the pancreas causes EPI, and results in symptoms of maldigestion and malabsorption of nutrients. Symptoms of celiac disease and EPI can be very similar, such as changes in the stool, and weight loss. According to the American College of Gastroenterology Clinical Guidelines on the diagnosis and management of celiac disease, patients with persistent gastrointestinal symptoms, signs, or laboratory abnormalities should be investigated for other causes, including EPI.
Announcer: This program was sponsored by AbbVie US Medical Affairs. If you missed any part of this discussion, visitReachMD.com/IndustryFeature. This is ReachMD. Be part of the knowledge.